DME & HME AI Automation
Clean claims start here
The solution DME and HME leaders trust to optimize their revenue cycles, from order to payment.
















The Standard of Trust
Why DME leaders keep choosing us, by the numbers.
auto-extracted from medical documents
on average within 12 months of go-live
across hundreds of HCPCs and dozens of payors

Your mission is patient care, not paperwork.
DME and HME providers deserve better than endless administrative struggles. Our industry-trusted AI solution verifies coverage requirements at intake and helps you build clean claims with automation—reducing your DSO, eliminating denials, and freeing your team from the administrative burden that's been holding you back.
Trusted AI. Proven Results. Built for DME.
Streamline order intake for respiratory, PAP, mobility, and medical supplies. Reduce denials and accelerate reimbursements with automated order intake and claim review. Learn More
Cut DSO and achieve 95%+ clean claims rates. Transform your revenue cycle efficiency with intelligent documentation processing and payor compliance checks. Learn More
Eliminate the constant challenges of staff turnover, recruitment costs, and offshore coordination. Handle peak season volumes without overtime or weekend work, while maintaining quality year-round. Learn More
Simplify complex documentation requirements and verify medical necessity for specialized treatments. Manage orders seamlessly to maintain continuous patient care and payment streams. Learn More
Feature highlights
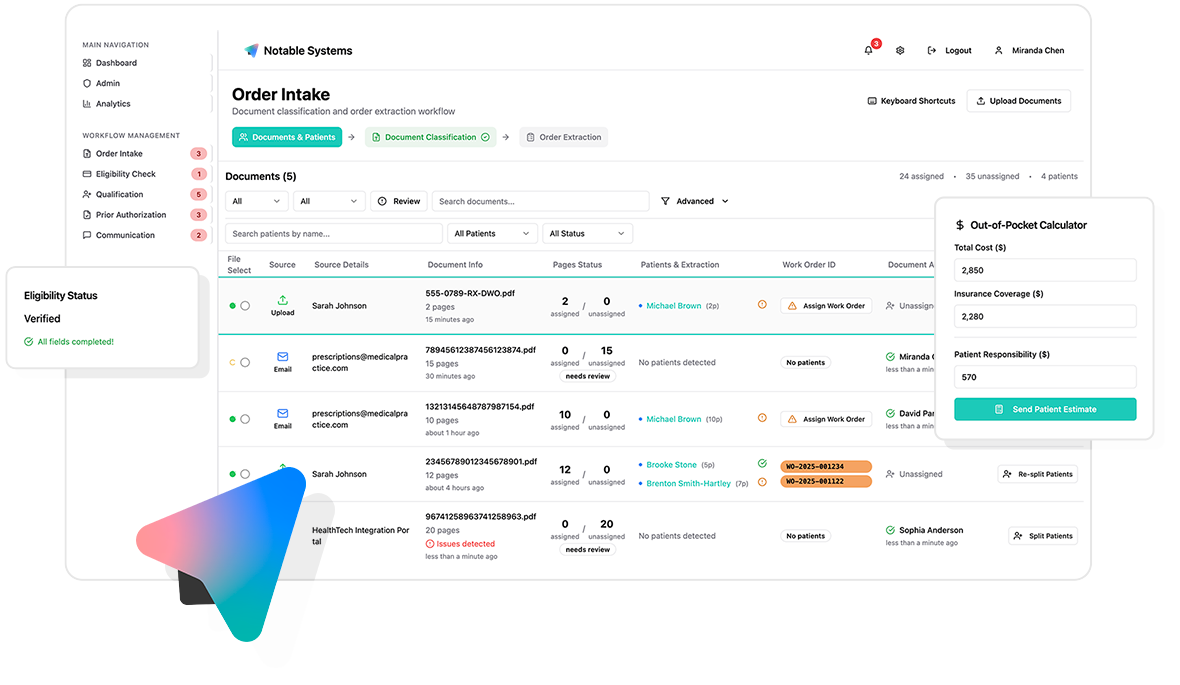
Document management
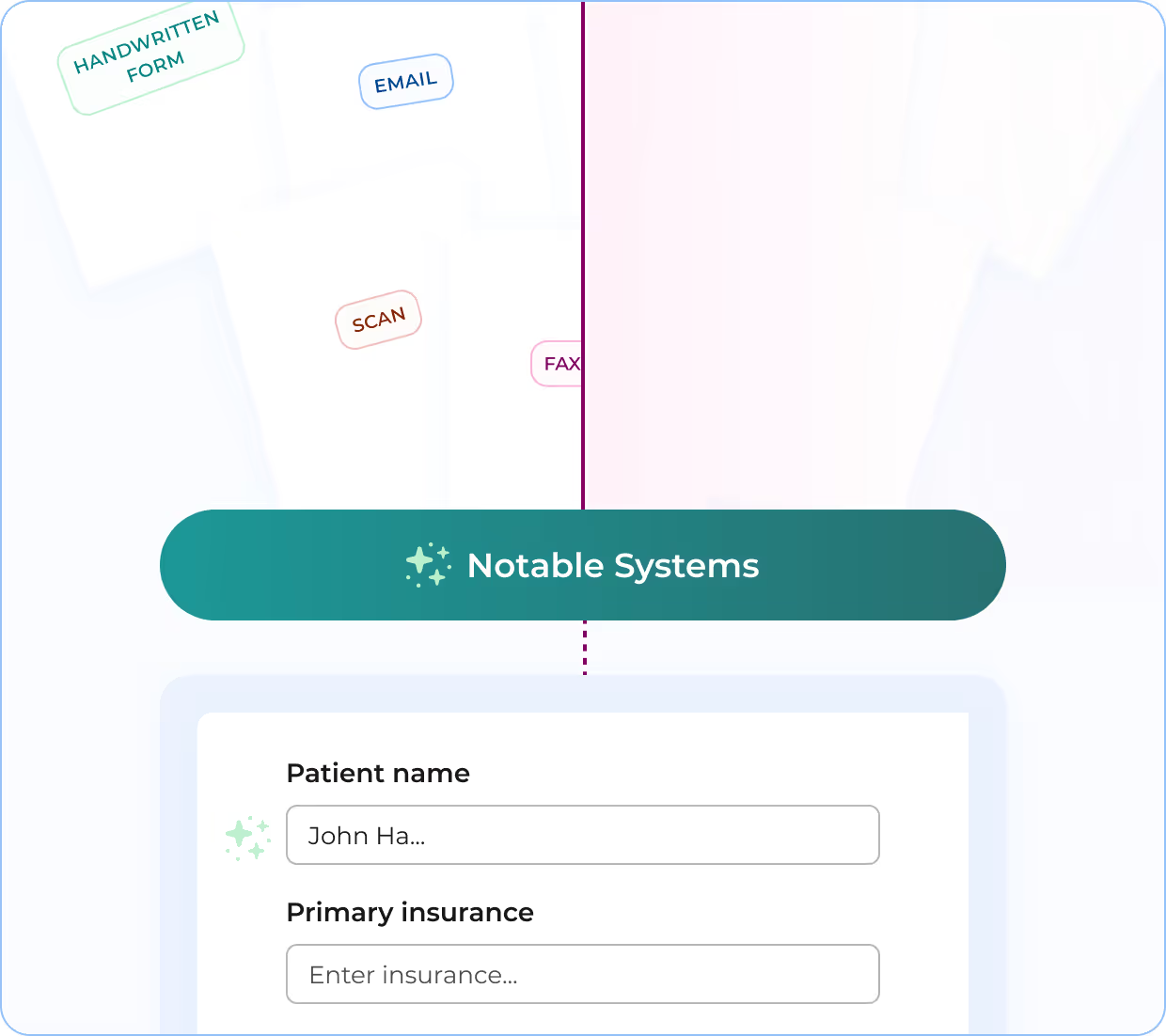
Eliminate manual document routing bottlenecks. Automatically ingest medical documents from any source through any channel, creating seamless workflows that process documents without human intervention.
Platform integration
Integrate seamlessly with NikoHealth, Brightree, and custom billing systems with ease. Deliver clean, structured data that flows directly into your workflows, eliminating manual data entry from intake to qualification and beyond.

Patient & order creation
AI automatically extracts key fields from incoming documents and applies custom business rules to create new patient accounts, generate orders, and update existing profiles. Our platform handles 100+ fields and 200+ rules as needed for your specific workflows.

Document standardization & classification
Transform chaotic, unstructured documents into clean, searchable PDFs. AI processes messy inputs—skewed scans, degraded faxes, mixed formats—then standardizes, classifies, and routes documents according to your team's requirements for compliant downstream processing.

Data validation & insights
AI-powered logic applies custom rules and quality checks to flag missing information, identify compliance issues, and surface business opportunities during document intake. Configurable validation ensures clean data flows to your billing systems.

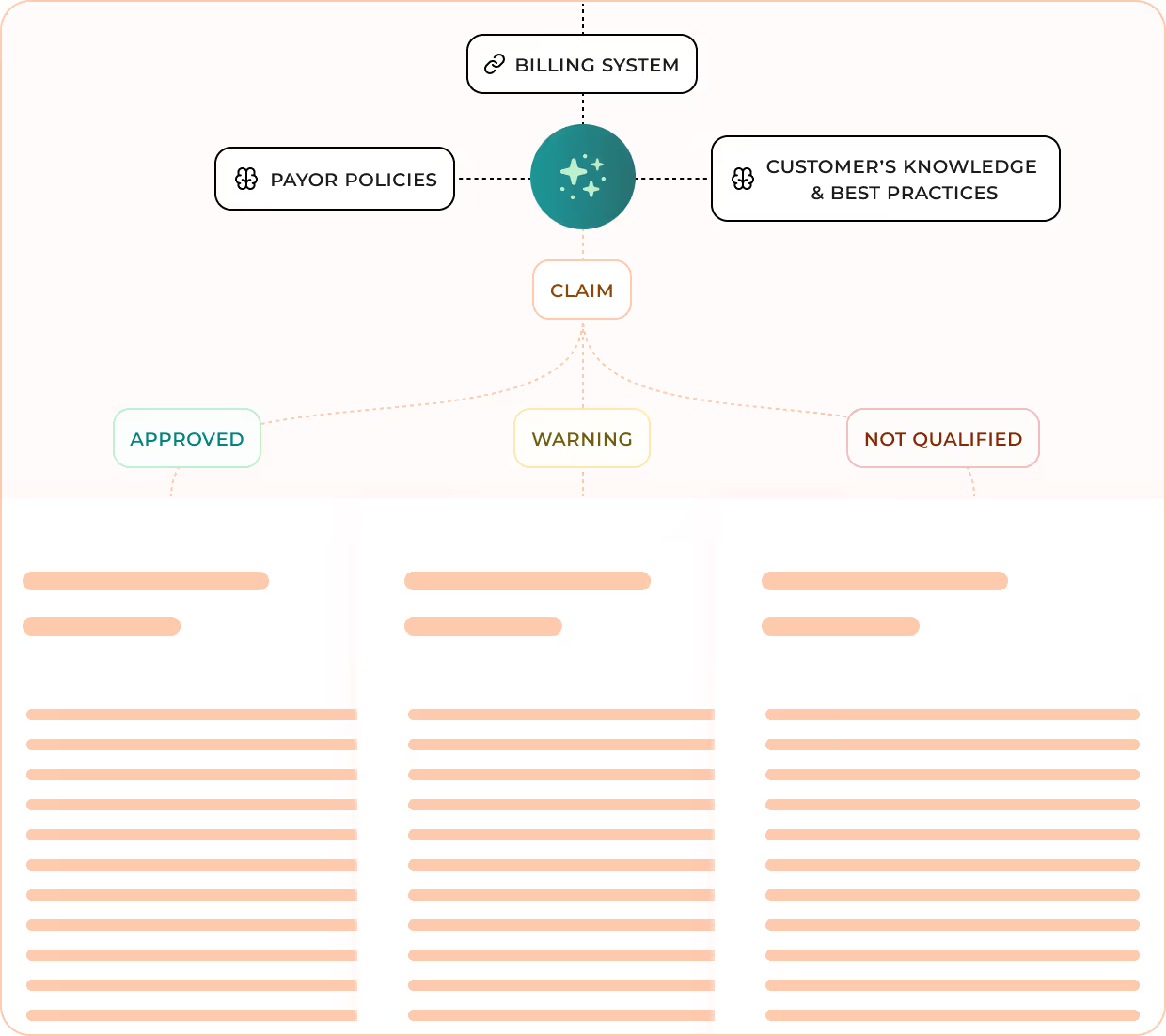
Pre-claim verification
AI evaluates orders against payor-specific coverage criteria before submission using our Payor Greenlight System (PGS). Trained by RCM experts with decades of experience, PGS provides clear pass/fail determinations within minutes, reducing denials and accelerating approvals.
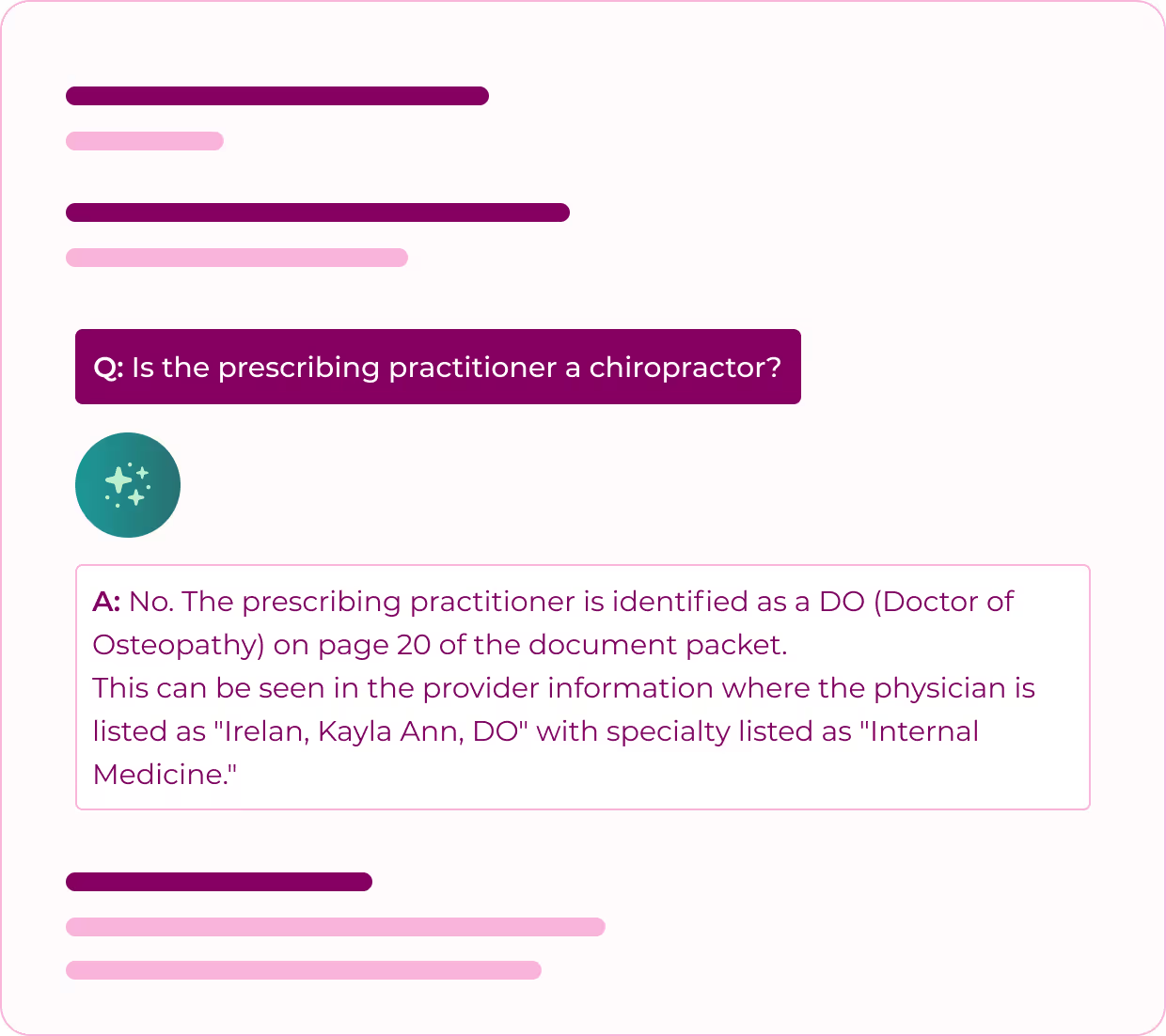
Detailed reasoning reports
Access comprehensive Q&A documentation showing the logical structure behind every claim determination. Hundreds of question-answer pairings provide complete transparency into model reasoning, delivering valuable audit protection and appeal support.
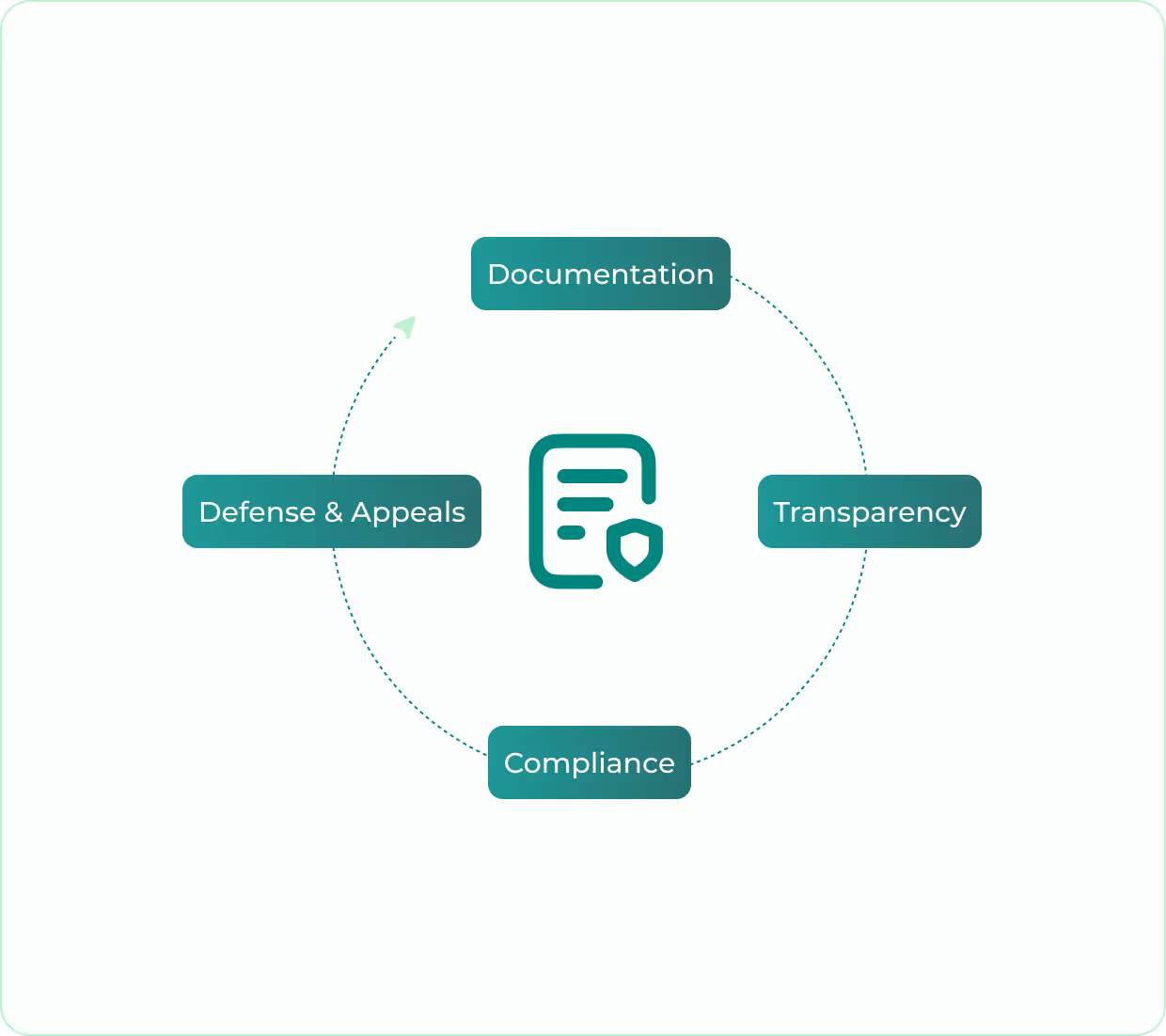
Audit & appeal support
Built to be the ultimate advocate for your reimbursement team. AI provides comprehensive documentation and transparent reasoning to defend claims during audits, strengthen appeals, and demonstrate compliance accuracy, helping accelerate processing and minimize write-offs.
See Notable
Systems in Action

See Notable
Systems in Action






Frequent asked questions
What is Notable Systems?
Notable Systems is the trusted AI automation partner for DME and HME leaders looking to eliminate their biggest revenue cycle headaches. Our technology reads faxes and complex paperwork, verifies claim accuracy before submission, and helps prevent surprise denials.
We support enterprise-scale operations with fully customized solutions, while also serving smaller providers through partnerships with NikoHealth, Brightree, and Valere Health. The result is less paperwork, fewer denials, happier staff, and stronger cash flow.
How much does Notable Systems cost?
Our pricing is customized based on your monthly document volume, product categories, and specific requirements. We offer transparent, usage-based pricing with no hidden fees or per-seat charges.
Contact us for a personalized quote.
Can you handle multiple product categories?
Yes, we support all major DME product categories including CPAP/oxygen, wheelchairs, orthotics, prosthetics, diabetic supplies, wound care, and more. If we don't currently support your specific category, we can build it out as part of our partnership.
Do you update payor rules automatically?
Yes, our team of DME industry experts continuously monitors LCD updates, payor policy changes, and regulatory updates. We update your rules automatically so you don't have to worry about staying current.
Are you HIPAA compliant?
Yes, we are fully HIPAA compliant and SOC 2 Type II certified. We maintain the highest standards for data security and privacy protection.






